B-Vitamins And Mood

Elevated Homocysteine Has A Strong Association With Poor Mood.
Homocysteine comes from the metabolism of certain foods we eat. When we are deficient in vitamins B6, B9 (folic acid) and B12, homocysteine may become elevated (1).
Elevated homocysteine has been linked to many issues, including poor mood (1)(2)(3).
Homocysteine’s association with poor mood has been noted as early as the 1970s (2). One study has even shown that in those tested, around 45-55% of people with low mood had elevated homocysteine (3). Elevated homocysteine is believed to impair the normal biological processes of the brain which researchers believe could explain its association with poor mood (3).
When It Comes To Folic Acid, Absorption Matters.
The MTHFR enzyme is responsible for converting folic acid (vitamin B9) to its biologically active form for use in the body. Mutations in the gene that produce this enzyme are relatively common (up to 40% of the population) (4). This may result in decreased absorption and benefit when taking folic acid that is not in it’s most active form, L-methylfolate (5).
A large analysis study that evaluated over 20,000 patient records found those with common defects of the MTHFR producing gene were at a statistically significant increased risk of developing issues related to mood (6).
Vitamins B6, B9 and B12 have also been shown to support improvements in concentration, memory, anxiety, stress and brain fog (7)(8)(9).
*Unlike most dietary supplements, Aquilegy only uses the biologically active forms of vitamins B6, B9 and B12 to ensure your maximum potential benefit.
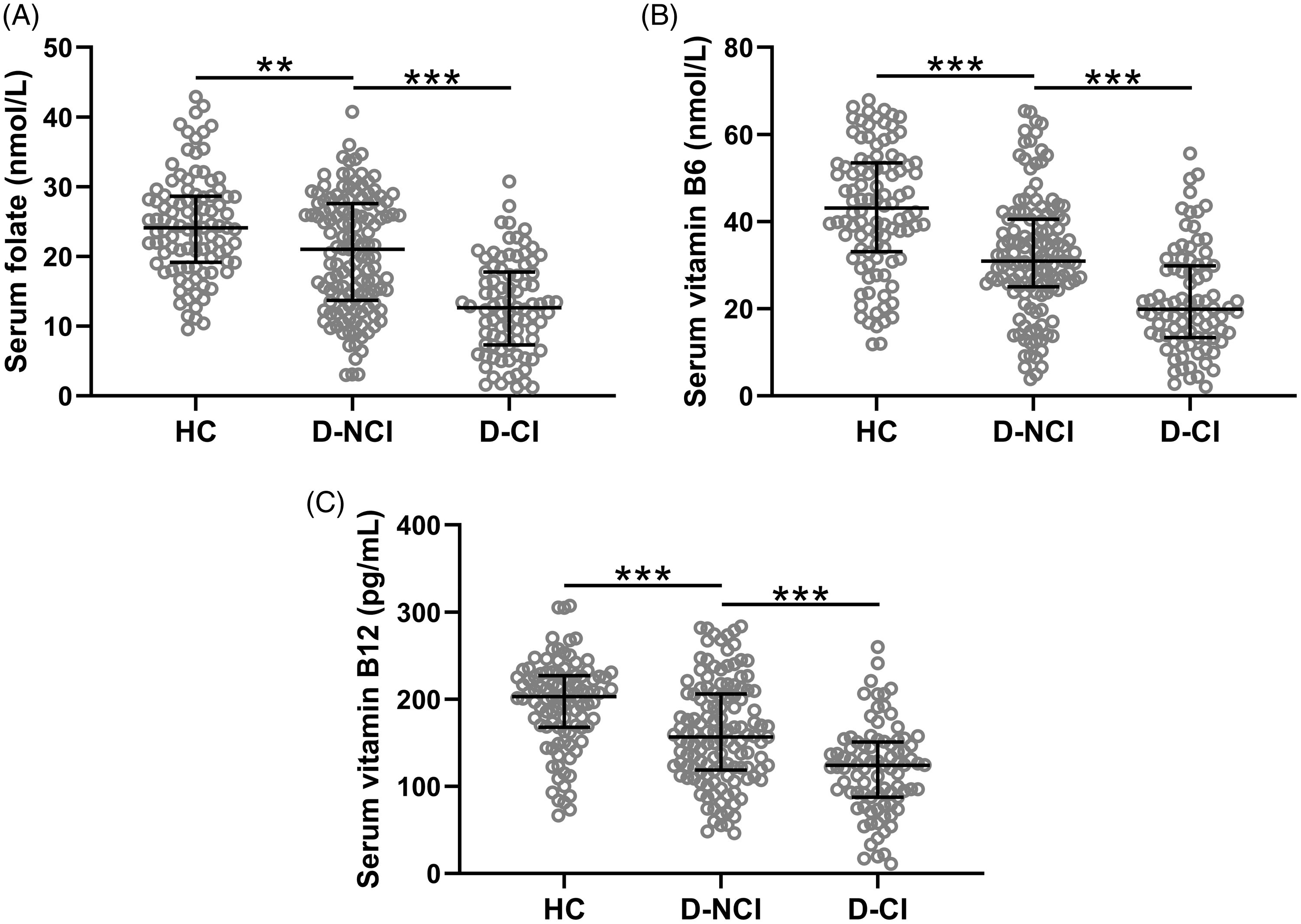
*(Zhao L, Guan L, Sun J, Li X. Serum levels of folate, vitamin B6, and vitamin B12 are associated with cognitive impairments in depression patients. Acta Neuropsychiatrica. 2024;36(1):44-50. doi:10.1017/neu.2023.41)

1) Folstein, M., Liu, T., Peter, I., Buel, J., Arsenault, L., Scott, T., &; Qiu, W. W. (2007). The homocysteine hypothesis of depression. American Journal of Psychiatry, 164(6), 861–867. https://doi.org/10.1176/ajp.2007.164.6.861
2) Reynolds, E. H., Preece, J. M., Bailey, J., &; Coppen, A. (1970). Folate deficiency in depressive illness. British Journal of Psychiatry, 117(538), 287–292. https://doi.org/10.1192/s0007125000193250
3) Karakuła H, Opolska A, Kowal A, Domański M, Płotka A, Perzyński J. Czy dieta ma wpływ na nasz nastrój? Znaczenie kwasu foliowego i homocysteiny [Does diet affect our mood? The significance of folic acid and homocysteine]. Pol Merkur Lekarski. 2009 Feb;26(152):136-41. Polish. PMID: 19388520.
4) Varga, E. A., Sturm, A. C., Misita, C. P., & Moll, S. (2005). Homocysteine and MTHFR mutations. AHA Circulation, 111(19). https://doi.org/10.1161/01.cir.0000165142.37711.e7
5) Vidmar Golja, M., Šmid, A., Karas Kuželički, N., Trontelj, J., Geršak, K., & Mlinarič- Raščan, I. (2020). Folate insufficiency due to MTHFR deficiency is bypassed by 5- methyltetrahydrofolate. Journal of Clinical Medicine, 9(9), 2836. https://doi.org/10.3390/jcm9092836
6) Peerbooms, O. L. J., van Os, J., Drukker, M., Kenis, G., Hoogveld, L., de Hert, M., Delespaul, P., van Winkel, R., &; Rutten, B. P. F. (2011). Meta-analysis of MTHFR gene variants in schizophrenia, bipolar disorder and Unipolar Depressive disorder: Evidence for a common genetic vulnerability? Brain, Behavior, and Immunity, 25(8), 1530–1543. https://doi.org/10.1016/j.bbi.2010.12.006
7) Jatoi, S., Hafeez, D. R. A., Riaz, S. U., Ali, A., Ghauri, M. I., &; Zehra, M. (2020). Low vitamin B12 levels: An underestimated cause of minimal cognitive impairment and dementia. Cureus. https://doi.org/10.7759/cureus.6976
8) Hughes, C., Ward, M., Tracey, F., Hoey, L., Molloy, A., Pentieva, K., &; McNulty, H. (2017). B-vitamin intake and biomarker status in relation to cognitive decline in healthy older adults in a 4-year follow-up study. Nutrients, 9(1), 53. https://doi.org/10.3390/nu9010053
9) Mahdavifar, B., Hosseinzadeh, M., Salehi-Abargouei, A., Mirzaei, M., &; Vafa, M. (2021). Dietary intake of B vitamins and their association with depression, anxiety, and stress symptoms: A cross-sectional, population-based survey. Journal of Affective Disorders, 288, 92–98. https://doi.org/10.1016/j.jad.2021.03.055